Acromegaly
You may look at that person up above and think one of two things:
1. “Whoa, he’s huge.”
2. “Meh, other wrestlers are better.”
Either way you take it, the Great Khali (pictured above), a fairly well known wrestler, is only this huge because of a specific medical condition that he has: Acromegaly.
And that is what we would talk about today.
Acromegaly is directly a result of excessive Growth Hormone production by the body. It’s literally in the name right? Growth Hormone = Excessive Growth. And that is essentially what Acromegaly is.
Let’s start by reviewing how Growth Hormone is usually regulated:
Regulation of Growth Hormone
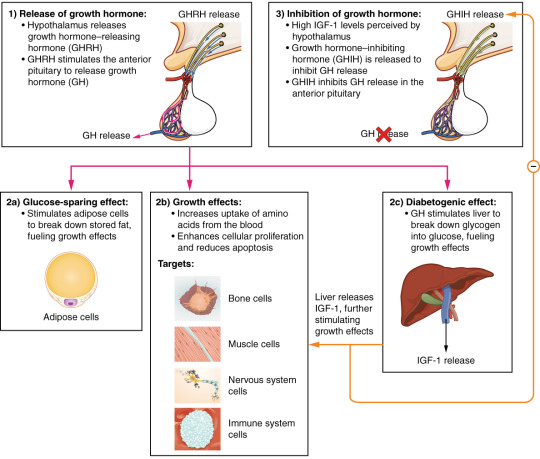
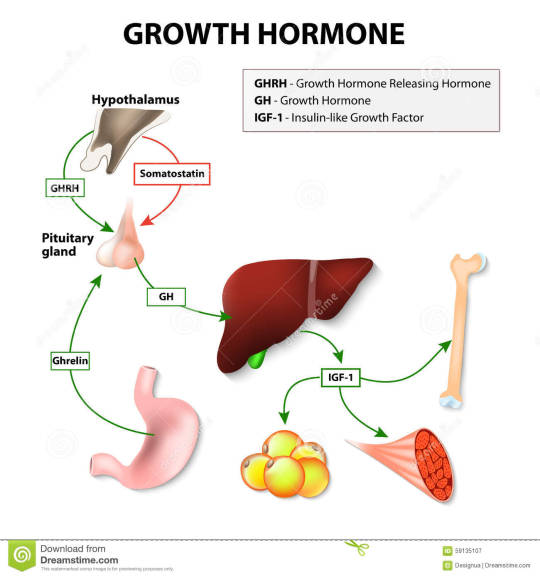
This is an excellent depiction of the simple way in which Growth Hormone is usually regulated. Growth Hormone is classically released by two different mechanisms:
1) Growth Hormone Releasing Hormone (GHRH)
2) Ghrelin
These are the two hormones that stimulate the production of Growth Hormone. GHRH is the far more classical of the two, and is a hormone that is released by the hypothalamus that directly stimulates the anterior pituitary to secrete Growth Hormone. GHRH is known to be released in a pulsatile manner – and thus Growth Hormone is released in a pulsatile manner. Take a look at the diagram below:
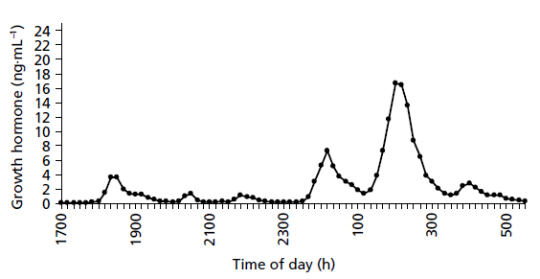
You can appreciate that the GH release is quite pulsatile indeed, and is highest between 1AM and 3AM in the night. This is reflective of the fact that GHRH is also released in a pulsatile manner.
The second hormone, Ghrelin is less understood (but honestly GHRH isn’t very well understood either). Ghrelin is released whenever the stomach is empty. Yep, it’s the hunger hormone. Somehow, this hunger hormone activates Growth Hormone release when it is very high. This is because Ghrelin is signalling that Growth Hormone release is necessary to allow the use of energy since the body is not achieving much energy from the food products it is consuming.
And this brings us to the functions of Growth Hormone:
Functions of Growth Hormone
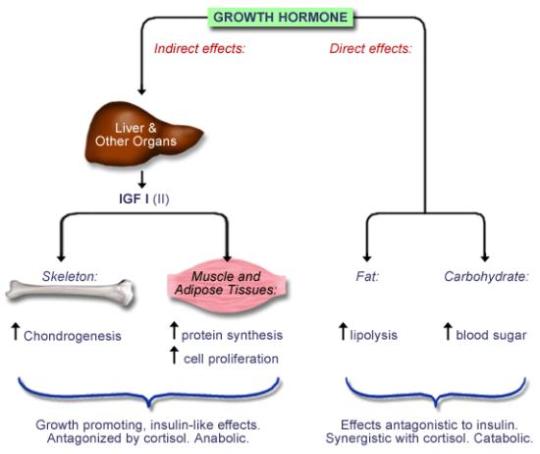
The effects of growth hormone on the body can generally be described in one word: anabolic (building up). Some of its effects are catabolic, but the more important effects are generally anabolic.
It exerts its effects through two major mechanisms:
- It promotes the activity of a pathway known as the MAPK/ERP Pathway, which causes chondrocyte proliferation and thus growth of cartilage.
- It causes the release of this very important compound, IGF-1 (insulin like growth factor 1), that basically acts as a stimulant for everything, causing growth of every receptor it gets into contact with.
Other than this, the major catabolic effect of Growth Hormone is promoting lipolysis – hence the reason Ghrelin would activate GH. So that the body can use the free fatty acids for energy in a time when the body is starving.
Also note that you can get an increased blood glucose in the body because Growth Hormone inhibits the body from using up the glucose stores.
All in all, the functions can be summarised as:
Great, now let’s get into Acromegaly, shall we?
What is Acromegaly?
Acromegaly refers to a condition that occurs when there is excessive production of Growth Hormone after the closure of the epiphyseal plates. This means that Acromegaly CANNOT happen in children since their epiphyseal plates are still open. In children, excess Growth Hormone results in a condition called Gigantism (which is pretty much the same thing as Acromegaly, but a little different), that we will discuss at another point in time.
So what could the most common cause of excess Growth Hormone be?
Easy.
A Growth Hormone producing adenoma accounts for 98% of all cases of Growth Hormone excess. And the most common place this adenoma occurs is the Pituitary Gland – hence 98% of causes of Acromegaly can be accounted for by a Growth Hormone Producing Pituitary Adenoma (also called a Somatotrope Adenoma). This type of adenoma accounts for 10% of all pituitary adenomas.
The majority of these somatotrope adenomas produce growth hormone alone, but you should also remember that some (about 25% of all somatotrope adenomas also produce excess prolactin – and so you get symptoms of Acromegaly AND Hyperprolactinemia.)
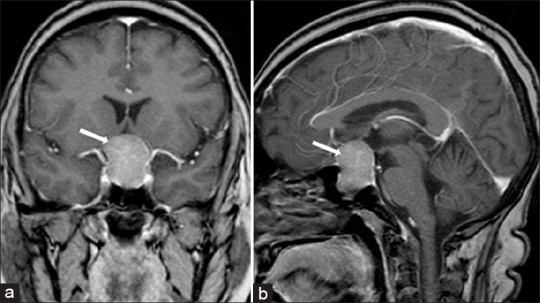
The MRI below shows a Pituitary Adenoma, that when combined with a history of Acromegaly is pretty diagnostic for a Pituitary Adenoma.
But other causes DO exist, albeit VERY rare. You can probably think of one based on what I gave you above.
A GHRH producing tumour of the hypothalamus. I just bolded this, but honestly you probably would never see this unless you’re a superspecialist or something of the sort because it is pretty rare (like less than 1% kind of rare). They happen very rarely as a result of things like a hypothalamic hamartoma and pancreatic islet cell tumours, but don’t count on it.
Clinical Features of Acromegaly
So really and truly, we can say that Acromegaly exerts 3 major categories of clinical features.
- Growth Related
- Since acromegaly causes excess production of IGF-1 which literally causes the growth of a number of tissues.
- The growth related effects can also now be divided into three further categories for even further simplicifcation:
- Hard Tissue Growth
- Arthralgia due to joint tissue overgrowth
- Enlarged jaw (macrognathia)
- Frontal Bossing
- Widened space between lower incisor teeth
- Increased hand and foot size.
- Soft Tissue Growth
- Increased heel pad thickness (and thus an increasing shoe size)
- Increased soft tissue growth of tissues of the fingers (and hence rings feel tighter)
- Coarsening of facial features.
- Skin tags
- Laryngeal Muscle Enlargement (which can result in sleep apnea and a hollow quality voice.)
- Carpal Tunnel Syndrome.
- Visceromegaly (Organomegaly)
- Macroglossia
- Hypertrophic Cardiomyopathy
- This is the most common cause of death in patients with Acromegaly.
- Fatal arrythmias and diastolic dysfunction leading to heart failure eventually develop.
- Hypertension also occurs due to the increase in resistance virtually in every organ and vessel since everything is becoming thicker.
- Thyromegaly
- Colonic Polyps
- It is for this reason that Growth hormone is associated with an increased risk of colon malignancy.
- Hepatosplenomegaly (But this is less significant than the above 4).
- Hard Tissue Growth
- Metabolic
- We already know that growth hormone causes an increase in blood glucose, and an increase in lipolysis. Surely this would have some sort of metabolic effects, no? Let’s look at them:
- Increased blood glucose level leading to diabetes mellitus.
- 25% of Acromegaly patients actually develop Diabetes Mellitus, and this is because remember, Growth Hormone is a counter-regulatory hormone that limits the effects of insulin and causes an increase in blood glucose – this is essentially insulin resistance!
- Hyperhidrosis (excessive sweating)
- Due to excessive growth and stimulation of the sweat glands.
- Acanthosis Nigricans (Think Diabetes Mellitus)
- Increased blood glucose level leading to diabetes mellitus.
- We already know that growth hormone causes an increase in blood glucose, and an increase in lipolysis. Surely this would have some sort of metabolic effects, no? Let’s look at them:
- Mass Effect
- We cannot forget that Acromegaly is mainly caused by a pituitary mass, and this mass would of course invade into surrounding tissues and cause damage. This is known as parasellar invasion.
- Headache
- Superior Spread leads to compression of the Optic Chiasm leading to bitemporal hemianopsia.
- Inferior Spread leads to sphenoid sinus invasion.
- Lateral Spread leads to Cavernous Sinus invasion.
- We cannot forget that Acromegaly is mainly caused by a pituitary mass, and this mass would of course invade into surrounding tissues and cause damage. This is known as parasellar invasion.
Despite all this, the clinical features of acromegaly are quite indolent, and will usually only appear about 10 years after the initial insult. Thus, in a case where a patient had Acromegaly AND Hyperprolactinemia due to a Somatotrope Adenoma that produces both, the symptoms of hyperprolactinemia would usually appear first and be much more prominent.
Diagnosis of Acromegaly
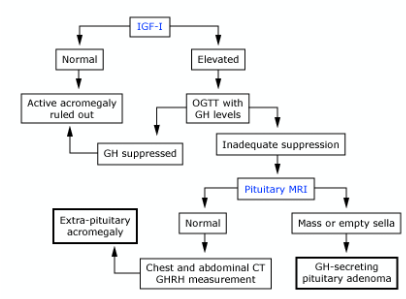
So let’s think about how we can diagnose Acromegaly. Let’s look at a little diagram:
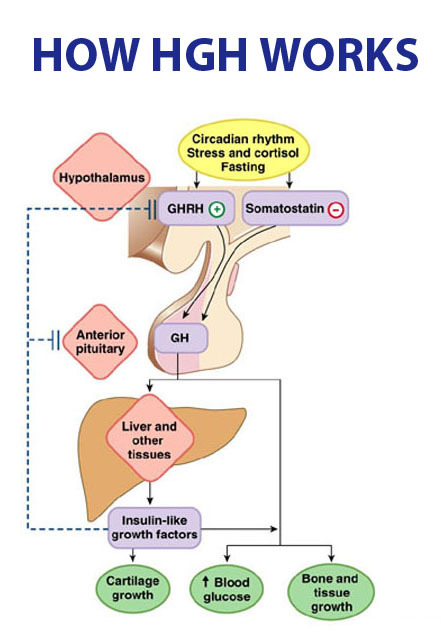
(You may notice something there called somatostatin – I’ll get into that in a bit).
So seeing how GH works, let’s try to brainstorm a few methods of checking for Growth Hormone excess.
The most obvious is measuring growth hormone right? The problem is that Growth Hormone fluctuates throughout the day, so if we were to measure growth hormone we would have to make a standard of the normal growth hormone level for every second of the day, and even then, some people have different patterns. This also applies to Growth Hormone Releasing Hormone, which is also a fluctuating pattern. This means we cannot use these.
Hence, the best test to screen for acromegaly is serum age matched IGF-1. IGF-1 does not vary throughout the day, because when it is produced by growth hormone, the fluctuating effect is negated by the fact that IGF-1 has a long half-life and thus would remain in the system. Furthermore, IGF-1 is produced exclusively by Growth Hormone, and thus is very accurate in representing the effect of Growth Hormone.
But serum IGF-1 is still not sufficient enough to fully diagnose Acromegaly – however it is a very useful screening test.
The diagnosis of Acromegaly is made using a OGTT (Oral Glucose Tolerance Test). Let me explain. Remember that Growth Hormone is one of the counter-regulatory hormones. So when a person consumes a large amount of glucose, the body would want to store away that glucose using insulin, and thus would decrease Growth Hormone production, since Growth Hormone directly acts against insulin. In Acromegaly however, the GH is being produced so constantly that the body is not able to shut down it’s production when it is given a glucose load. So this means that in acromegaly, the growth hormone levels fail to decrease to a value that <0.4ug/L after being given a 75g dose of glucose. This means that the value of GH remains elevated >0.4ug/L after being given the 75g glucose.
After you have established that there is indeed acromegaly somewhere, you have to find out where is the acromegaly coming from? Naturally, since the most common cause is a pituitary adenoma, the next step after this is a pituitary MRI to confirm the GH producing pituitary adenoma.
This is quite unlikely, but if the MRI is normal, then you can do an abdominal and chest CT to examine for extra-pituitary sources of acromegaly, or do a GHRH level to examine for a hypothalamic etiology.
Do not forget that it may also be relevant to perform tests to monitor organs once the diagnosis of Acromegaly is made. These include little tests like Thyroid Function Tests for thyromegaly, Echocardiograms for the Hypertrophic Cardiomyopathy, Endoscopy for colonic polyps and HbA1c for monitoring Diabetes Mellitus (among many others).
Other laboratory abnormalities in acromegaly include:
- Elevated triglycerides and free fatty acids
- Due to increased lipolysis
- Elevated prolactin (if the adenoma also produces prolactin).
- Hyperphosphatemia
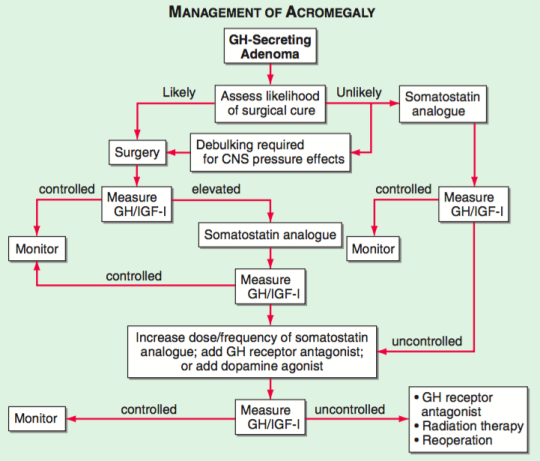
Treatment of Acromegaly
Now let’s think back about how we can treat acromegaly. The very first thought we can have is that acromegaly is produced as a result of (98% of the time) a pituitary growth hormone producing adenoma. The easiest solution?
But no, seriously speaking, transphenoidal resection of the pituitary adenoma is the first line treatment almost all cases of acromegaly.
The other option to think about is somehow inhibiting Growth Hormone Production. Thankfully, the body has a hormone that can do this. Remember how I mentioned something known as somatostatin above? Yep, somatostatin inhibits the production of Growth Hormone. This means that another viable alternative is to use somatostatin analogues, such as octreotide.
Other second line options include Growth Hormone Releasing Hormone Antagonists (such as pegvisomant) which would inhibit binding of the growth hormone to its receptor, and high dose dopamine agonists which are a last resort for reducing growth hormone production (such as bromocriptine and cabergoline -which are incidently the first choice method in treating a prolactinoma).
Radiation therapy is also an option, but these really are last line options that should come after Surgery and Octreotide.
That’s it for Acromegaly guys! Congrats on making it to the end! If there are any questions you can always PM me and I’ll reply.
Videos:
https://www.youtube.com/watch?v=1MJTkz02SaM
Questions:
1. A 23 year old man complains of a persistent headache. He has noticed gradual increase in his ring size and shoe size over the years. On physical examination he has a deep, hollow-sounding voice and a prognathic jaw. Visual studies suggest bitemporal hemianopsia. What initial study is indicated?
A. Serum IGF-1 and serum Prolactin
B. Morning Growth Hormone Levels
C. Dexamethasone Suppresion Test
D. Pituitary MRI
E. Oral Glucose Tolerance Test
2. A 24 year old female with an elevated IGF-1 and positive glucose tolerance test was studied using a pituitary MRI. However, the MRI revealed no adenoma. What is the next step?
A. Discharge the patient. She does not have acromegaly.
B. Counsel the patient on the normalcy of her physiological variant.
C. Investigate for Growth Hormone doping.
D. Perform a pituitary CT.
E. Perform an Abdominal CT.
Answers:
1. A
B. E


Hey, amazing article but can you explain this joke with treatment of acromegaly, that picture. Please. Thanks
LikeLike
Thanks for your nice work , From Cairo , Egypt .
LikeLike